Janet Macleod from Positive Art Therapy recently interviewed me, asking about my role as an art therapist. I enjoyed thinking about her questions and taking the time to answer them. After 14 years of practice, they gave me pause. I'm including the interview here as a record of my thoughts at this point in my career.
 Q: What motivated you to become an arts therapist?
Q: What motivated you to become an arts therapist?
I knew that I wanted to use art as a form of healing when I graduated from college but I didn’t become aware of art therapy as a field of study until my forties. By then, I was a professional artist and a mother. I’d had occasions to use art as a healing tool with my own children and in the studio art classes I taught. I was interested not so much in the technical aspect of art but rather what made someone draw and what those drawings might mean. I wanted to help people solve life problems with art and I needed formal training to do this. In a moment of serendipity, a lime green flyer arrived in the mail, advertising the Post Master’s Art Therapy Certificate program at UC Berkeley. Kismet!
Q: Where did you train? What is your most memorial experience while training – good or bad?

I have an MFA in sculpture and textiles from California Collage of the Arts, so the UC Berkeley postmaster’s certificate program was a great fit. During my internship, one of my most memorable events occurred while I was facilitating a children’s bereavement art group. I was fortunate enough to be hired as a student—and that meant I was learning on the job. I had heard my art therapy teachers’ horror stories about paint and clay splashed rooms, but I did not know much about containment, timing or allowing clients to maintain their defenses. One evening, I asked a group of teens to write a letter to their deceased. That evening was the first of a ten session group and after the exercise, one of the group members left the room and punched a hole through the wall! It was a powerful way of learning containment, timing and allowing clients to maintain their defenses.
Q: Who has most inspired you or influenced your work as an arts therapist?
When I began my internship (here at UC Davis Children’s Hospital), my supervisor, Johanna Russell was a great source of information and inspiration. I was full of art therapy theories but Johanna had been practicing for 10 years and knew the lay of the land. She also understood my perceived need for control in an uncontrollable environment. Over and over, she reminded me to “go with the flow,” words which have helped me to understand that even if I am organized, my materials at hand, ready to do an intervention, the patient might be anywhere other than where I expect them to be; at a procedure, playing foosball or heading to the cafeteria for a bite to eat. And that has to be ok.

Q: Are you employed as an arts therapist?
I work as a pediatric art therapist for UC Davis Children’s Hospital in Sacramento, CA.
Q: What populations do you predominantly work with?
Our Children’s Hospital contains the neonatal intensive care unit, the pediatrics unit and the pediatric intensive care unit. I work with children and their parents on all of those floors, but primarily on pediatrics. I also facilitate an art therapy bereavement group at UC Davis Hospice; designed by myself and Don Lewis, LCSW of UC Davis Hospice. The group is collaboration between the UC Davis Children’s Hospital and UC Davis Hospice.
Q: Where or who you really like to work with?
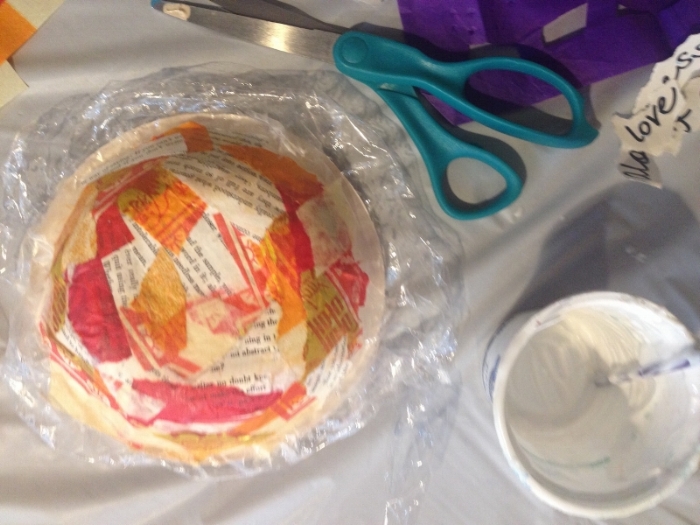
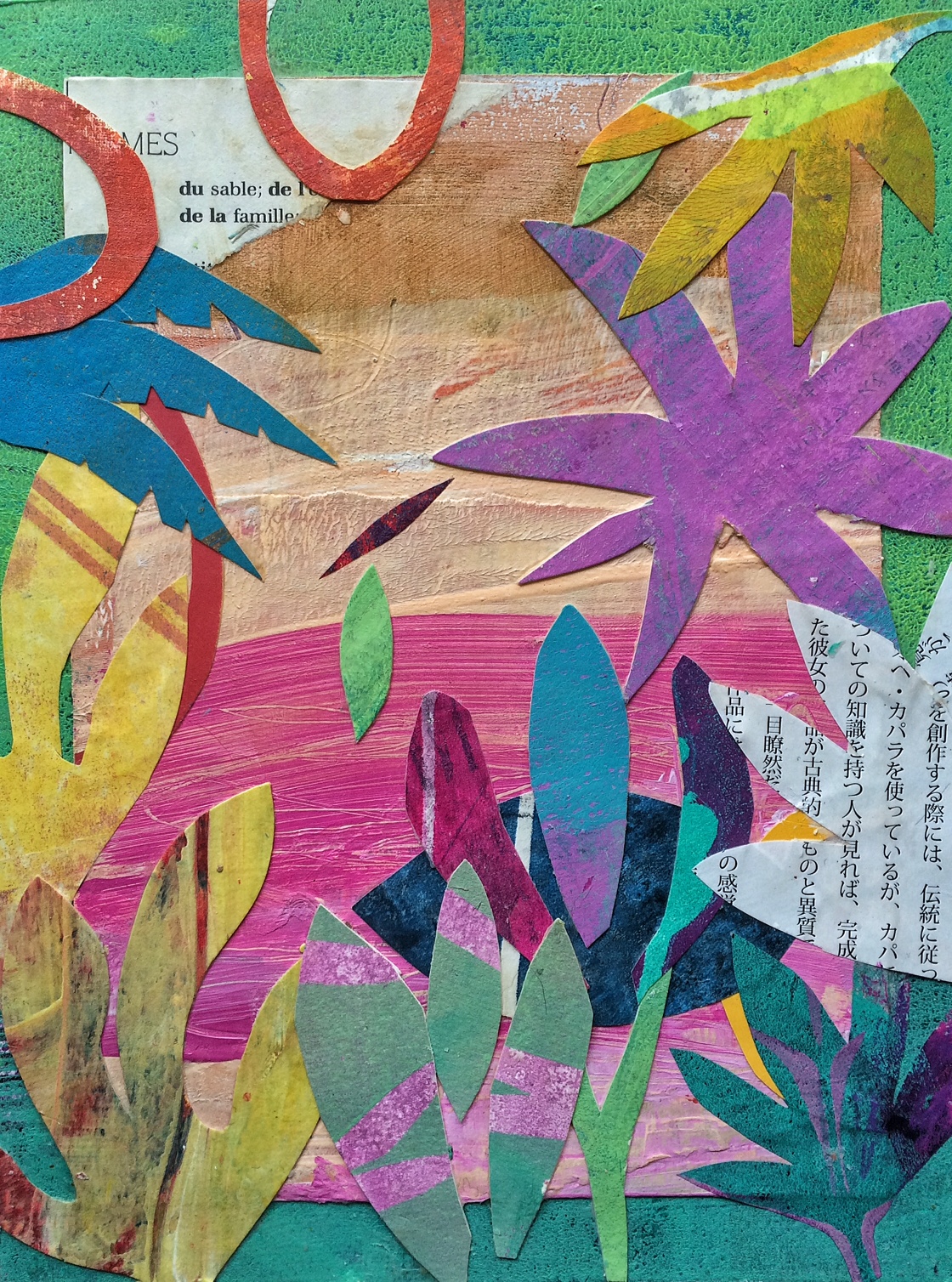
Hands down, our daily Art Therapy Group on the pediatric floor. I’ve been doing it for close to 14 years now and I love coming up with new ideas, new projects, new ways to interest children and families in art making. Kids come pulling IV poles, in wheelchairs or even carried by a parent. The group is huge source for normalization and socialization. Most people are surprised and delighted to find art in the midst of the hospital setting. Facilitating the Young Adult Bereavement Art Group is a close second. These young adults come from every imaginable background with every possible kind of loss. The ability to hold the group and see the changes in group members over the 8 week span is heartbreaking, heartwarming and inspiring.
Q: Do you practice your own art? If so what and who has influenced you?

Absolutely. I spend as much time as I can in my studio. I’m influenced by so many artists, but my current favorites are Giorgio Morandi, Pierre Bonnard, Milton Avery, and many Northern California artists. I’m also in love with the 18th century French still life painter, Jean-Siméon Chardin.
Q: What other interests do you enjoy when you are not working?
I’m passionate about art making, I love to practice yoga and I enjoy getting out and walking—whether it’s in our town or out on a trail. One of my favorite soothing activities is diving into a good book.
Q: What has been your biggest challenge while training or working as an arts therapist?

UC Davis Medical Center is a university hospital committed to learning as part of the healing process. Residents, interns and student nurses come to the hospital to learn. As an art therapist, learning as much as one can about the different diagnoses is of immense benefit to working with patients. I think of each illness or trauma as a kind of narrative, a story. The more I know about any particular narrative, the better I can assess each child’s circumstances. Considering the personality of the child, the family system and the illness becomes a puzzle to solve. When I can put my fingers on just the right art intervention, the results are worth the challenge of learning all of the medical terminology.
Q: What keeps you motivated?
There are many moments of joy and wonder. The presence of art in our setting is like magic. Children lying prone sit up and begin painting. A teen that has hidden under the blanket pokes her head out and starts to paint a watercolor. The knowledge that I’ve been created a pocket of goodness and delight during a time of illness or injury makes me very happy. I also draw tremendous strength from making art and from my family and friends.
Q: What is on your “wish list” either for yourself as an arts therapist or for the profession?

I have been active in the area of grief and loss since I began practicing art therapy, both in the hospital and in hospice. My biggest wish is that our Pediatric Palliative Care program will be able to grow by helping people to understand what palliative care really is. It is not a death sentence, but a way of caring for children with a chronic illness. Palliative care begins with the diagnosis, and addresses the physical, emotional, intellectual and spiritual effects of the disease on the child. A pediatric palliative care program provides that child and their family with the resources they need not only to cope, but to live a rich and fulfilling life whether that life is foreshortened or, they are able to live out a full lifespan.
Q: What strength do you have that has been most valuable to you as an arts therapist?
I’m able to act quickly on a referral, drawing on my intuition and improvisational skills to come up with a directive that targets the specific needs of the child.





 Q: What motivated you to become an arts therapist?
Q: What motivated you to become an arts therapist?




